The Heart of Behavior Integration
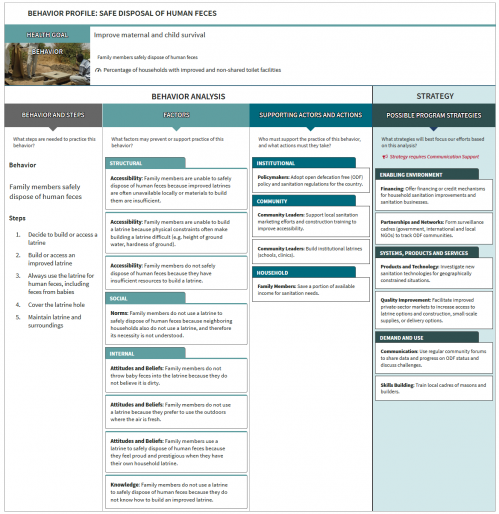
A Behavior Profile is an insight-driven way to analyze a specific behavior. The goal? Find evidence-backed routes to make smart program choices and nurture the changes you want to see in the communities you care about. 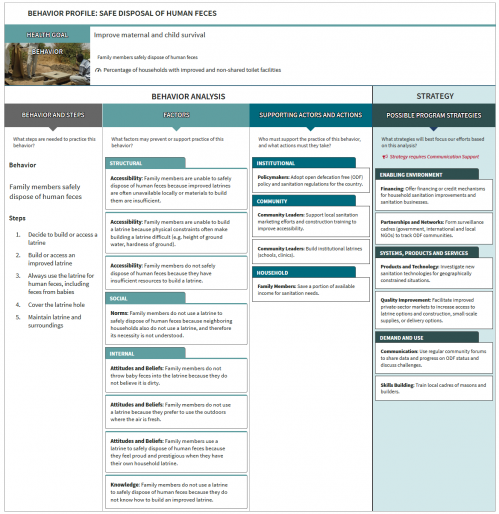
It’s just one tool in phase one of the Think | BIG process: Focus and Analyze. After you identify the behaviors most closely linked to your development goal, you create a Behavior Profile for each priority behavior.
Read on below for more details on:
- what developing a Behavior Profile involves,
- why a Behavior Profile is so important,
- when you use Behavior Profiles during your program,
- who can use Behavior Profiles, and
- how we help you build your own Behavior Profiles.
If you’re intrigued by the power of Behavior Profiles, check out an example Behavior Profile.
Or maybe you’ll have more fun learning how to develop a Behavior Profile and help a mother save her son: play the Behavior Profile Game
Need a refresher on a finished Behavior Profile? Or new to BIG and want to see real examples? Browse Behavior Profile samples, from nutrition, to gender-based violence, to environment and more.
When you are ready to take the plunge and develop your own Behavior Profile, we’re here to support you.
 Behavior profiles are at the heart of Thinking BIG.
Behavior profiles are at the heart of Thinking BIG.






 The Manoff Group was acquired by JSI in 2022.
The Manoff Group was acquired by JSI in 2022.